The Future of Healthcare Staffing Isn’t Remote. It’s Responsible.
Healthcare leaders don’t need another trend to chase.
They need staffing models that actually hold up under pressure.
Across the industry, the challenges look remarkably similar. Patient volumes continue to rise. Documentation requirements expand every year. Prior authorizations slow care delivery. Bilingual communication is inconsistent. And non-clinical turnover remains stubbornly high.
Most organizations respond the same way: post more jobs, raise wages where they can, and hope the next hire sticks.
For a growing number of physician-led healthcare systems, that approach is no longer enough.
Not because leaders aren’t trying hard enough, but because local labor markets alone can’t absorb the administrative load modern healthcare creates.
Why Physician-Led Systems Feel This First
Physician-led organizations sit at an intersection most systems don’t.
Clinical leaders are also operational leaders. When staffing breaks, they feel it twice — once in the exam room and again after hours, finishing charts or clearing inboxes that are never quite empty.
Burnout, in this context, isn’t abstract. It shows up as:
- Documentation spilling into nights and weekends
- Delays in patient communication
- Leadership time pulled away from care and growth
- A constant sense that the system is running just slightly behind
This isn’t a culture issue.
It’s a capacity issue.
And more physician-led systems are acknowledging a difficult truth: the traditional, local-first staffing model was never designed for this level of administrative complexity.
The Breaking Point of Local-Only Staffing
Local hiring still matters. It always will. But relying on it exclusively creates real constraints.
Hiring cycles stretch longer.
Turnover creates retraining fatigue.
Bilingual talent is harder to find and harder to retain.
One resignation can destabilize an entire workflow.
Even well-run practices find themselves reacting instead of planning, filling gaps instead of building durable capacity.
Over time, leaders start asking a different question:
What if the problem isn’t how fast we hire, but how we design staffing in the first place?
That question is driving a shift.
Beyond “Remote”: What Responsible Global Staffing Actually Means
There’s a reason many healthcare leaders hesitate when global staffing enters the conversation. For years, it’s been framed as a blunt instrument: cheap labor, minimal integration, unclear accountability.
That model deserves skepticism.
But what’s emerging now looks very different.
Responsible global staffing isn’t about outsourcing tasks and hoping for the best. It’s about intentionally integrating dedicated professionals into existing teams, workflows, and standards with compliance, continuity, and accountability built in.
It prioritizes:
- Role clarity over task dumping
- Long-term team integration over short-term cost savings
- Bilingual, healthcare-experienced professionals
- Systems that support documentation and communication in real time
In other words, it’s not “remote for remote’s sake.”
Its flexibility is designed for regulated, human-centered environments.

One physician-led system that recognized this early was DHR Health.
DHR Health: Proof of a Broader Shift
Like many healthcare organizations, DHR faced persistent recruiting and retention challenges in non-clinical roles.
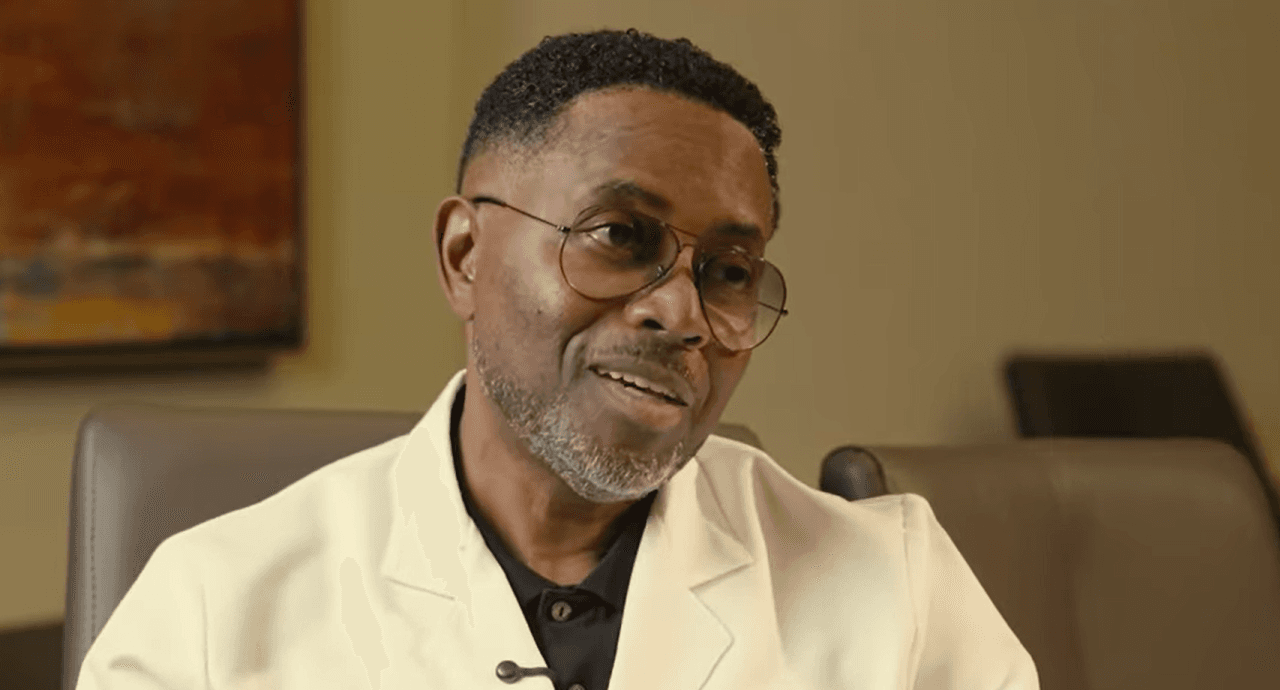
“We had a hard time like anybody else recruiting employees and retaining employees. We did not have enough staff,” shared Dr. Marcel Twahirwa.
The issue wasn’t a lack of effort. It was the limits of the local labor market.
Instead of doubling down on the same approach, DHR expanded its staffing strategy. They integrated dedicated global professionals to support administrative and operational functions — not as temporary help, but as part of the team.
That distinction mattered.

“We actually do not consider them to be Edge employees,” Dr. Twahirwa explained. “We consider them to be our own employees.”
That mindset shift (from outsourcing work to integrating people) is where many staffing initiatives succeed or fail.
What Changed When Capacity Was Redistributed
The impact at DHR wasn’t about flashy transformation. It was about stability.
Administrative work stopped bottlenecking care.
Documentation was completed during patient visits.
Messages moved faster.
Prior authorizations stopped lingering.
Most importantly, the weight physicians carried quietly began to lift.
“It reduced my mental stress,” Dr. Twahirwa said. “I’m relaxed now when I see my patients.”
That’s not a wellness program.
That’s an operational outcome.
Burnout didn’t disappear because physicians became more resilient. It eased because the system stopped asking them to absorb work that could be handled elsewhere.
Why This Model Is Gaining Momentum
Financial efficiency often enters the conversation, and it did at DHR.
“Better quality for cheaper than you will pay here,” Dr. Twahirwa noted.
But cost wasn’t the driver. Continuity was.
Reliable support.
Bilingual communication.
Teams that stayed, learned workflows, and improved over time.
That’s why this model is resonating with physician-led systems in particular. It doesn’t replace local teams. It reinforces them by removing the pressure points that cause burnout, churn, and operational drag.
Where Healthcare Staffing Is Headed
Over the next decade, healthcare operations will increasingly be shaped by a few realities:
Administrative work isn’t shrinking.
Patient expectations around access and communication are rising.
Local labor markets will remain constrained.
Organizations that respond by hiring reactively will continue cycling through the same challenges.
Organizations that adapt will design staffing systems that are:
- Flexible without being fragmented
- Global without being impersonal
- Compliant without being rigid
They won’t talk about “remote teams.”
They’ll talk about capacity, continuity, and care.
A Proof Point, Not a Pitch
After more than three years working with dedicated global team members, Dr. Twahirwa’s recommendation is simple:
“I would definitely recommend Edge… Edge is the company to go with.”
Not because it’s trendy.
Not because it’s novel.
But because it works — quietly, consistently, and sustainably.
That’s ultimately where healthcare staffing is moving. Away from location-based assumptions. Toward responsible, flexible systems that support physicians, protect patients, and allow healthcare leaders to build for the long term.
Not remote.
Responsible.
Interested in learning more about how Edge can advance your healthcare practice? Book a demo.